Breast cancer-associated LYMPHEDEMA prevention and treatment
Definition
Accumulation of protein rich fluid in interstitial space due to disruption of lymphatic circulation.
Lymphedema is a relatively common and often feared complication of breast cancer surgery
Lymphedema is also associated with an increased incidence of recurrent episodes of cellulitis with potentially life-threatening consequences.
Prevention and Early detection is key to management

Incidence
Highest incidence during 1st year Post-operative.
20-50% CA Breast survivors eventually develop lymphedema
80 % BCRL patients within first 3 years
1% Life long risk per year
Risk remains at 4-7% even after the shown success of SLNB
Patho-physiology
- Essential for maintaining body’s homeostasis, immune response, transportation of nutrients, and waste products.
- Hydrostatic pressure in arteries pushes the fluid into the interstitial space to provide nutrients to the surrounding tissues.
- 90% of interstitial fluid returns to circulation normally.
- Remaining 10% of interstitial fluid contains high molecular weight proteins ie large to enter capillaries.
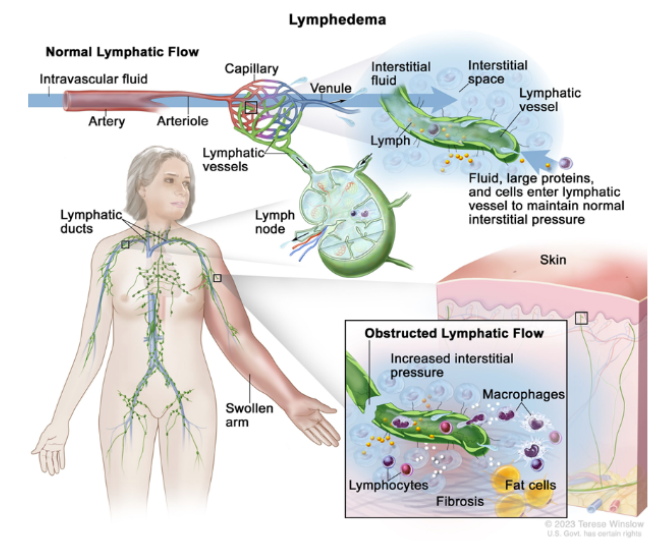
Lymphatic capillaries lack Basement Membrane therefore, they can absorb large particles.
Lymphatic capillaries- Large collecting Vessels They have Basement Membrane+ contractile pericytes and they possess valves which facilitate the lymph flow to Lymph Nodes circulation
- When lymph vasculature is injured due to surgery, the vessels are unable to transport the protein rich fluid to/from interstitial space( accumulation of protein in the space)
- Increased oncotic pressure; draws additional water to interstitial space.
Clinical Presentation
Swelling with pitting oedema at this stage
Prolonged stagnation of protein rich excess Interstitial fluid Leading to chronic inflammation and progression of lymphedema
Eventually leads to the inflammatory cascade and fibrotic changes in lymphatic vessels and surrounding soft tissues.
Accumulation of Interstitial Fluid activates the differentiation and proliferation of adipocytes.
Leading to adipose deposits OR massive adipose tissue hypertrophy
At the end increase in volume of extremity is noted by excess fat.
Diagnosis
Stage 0
- Swelling not evident
- Impaired Lymphatic drainage
- Changes in imaging
Stage I
- Clearly visible soft tissue pitting edema
- Swelling reduced by elevating the arm
Stage II
- Increased fibrosis, excess fat
- Pitting not detectable
- Swelling not reduced by elevation
Stage III
- Extreme swelling
- Fibrotic hard tissues
- Non-pitting edema
- Skin changes (blisters etc)
Risk Factors
- Extent of Surgery
- Extent of Local Surgery
- Radiation
- Obesity
- Genetic Susceptibility
- Infection
Extent of Surgery
Any kind of surgery ± radiation, has a risk of lymphedema
ALND: strongly shows BCRL (all might not develop lymphedema)
SNB: has reduced the incidence, but the risk still persists
E.G Anatomical variations, the existence of alternative lymphatic pathways: Cephalic Pathway draining into suprclavicular Lymph Nodes.
The tricipital pathway draining into posterior scapular nodes.
Extent of Local Surgery
Mastectomy: Increased risk of lymphedema
BCS Decreased risk of lymphedema
Radiation
Exact mechanism is not known but, it has been suggested that XRT Induced soft tissue fibrosis contributes to lymphedema
It also decreases the number of dermal capillary lymphatic vesseles and lymphatic endothelial cells, further adding to dysfunction.
Obesity
- Being over weight at the time of BCA Diagnosis is also one of the reasons for lymphedema
- BMI > 30 kg/m 2 has nearly 3 folds increased risk of lymphedema as compared to BMI < 25kg/m 2
- Obesity itself impairs the lymphatic flow
Infection
Lymphatic drainage is important for immunity, damage to this weakens the protection against infections leading to lymphedema.
Signs and Symptoms
Early Signs
- Slight puffiness
- Feeling of fullness
- Indentation from jewellery
- Swelling might subside during night
Persistant Symptoms
- Chronic lymphedema
- Pitting not detectable
- Size discrepancy of the arms
Imaging Techniques
Lympho-scintigraphy
Contrast Enhanced Magnetic Resonance Lymphangiogram (MRL)
Indocyanine Green Lymphography
Prevention
Patients should be informed about the early symptoms of lymphedema and encouraged to seek treatment as soon as they recognize these early signs.
They should be advised about proper skin care and to avoid infections.
Sentinel node biopsy
Level 1& 2 dissection
3 if level 2 is involved
Arm & shoulder exercises
Non Surgical Treatment
As soon as symptoms start to develop, conservative treatment should be started which helps to prevent irreversible tissue damage
General Measures
- Obese Patients: Weight loss, refer to dietician
- Patient with normal BMI: Encourage to avoid weight gain
- Adequate Hygiene: Skin care to avoid cracking and infections that may aggravate lymphedema.
- blood pressure measuring or blood sample taken from the ipsilateral arm have been advocated, although there is no evidence supporting these practices
- Flexibility Exercises:
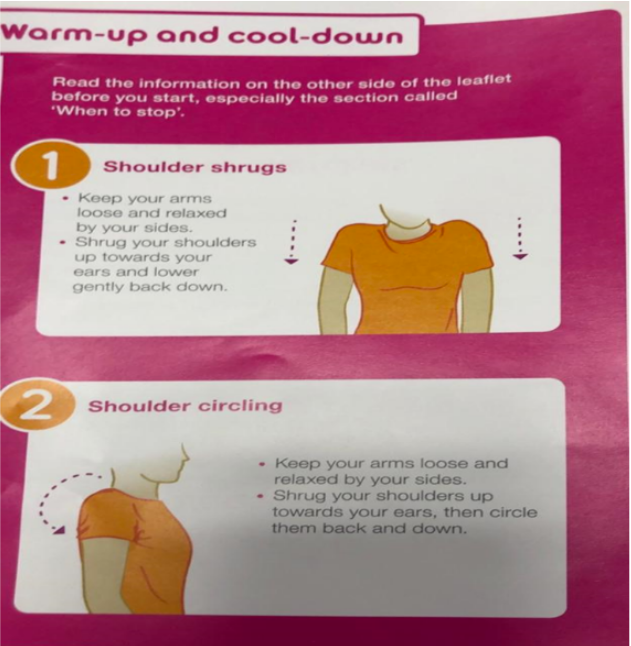
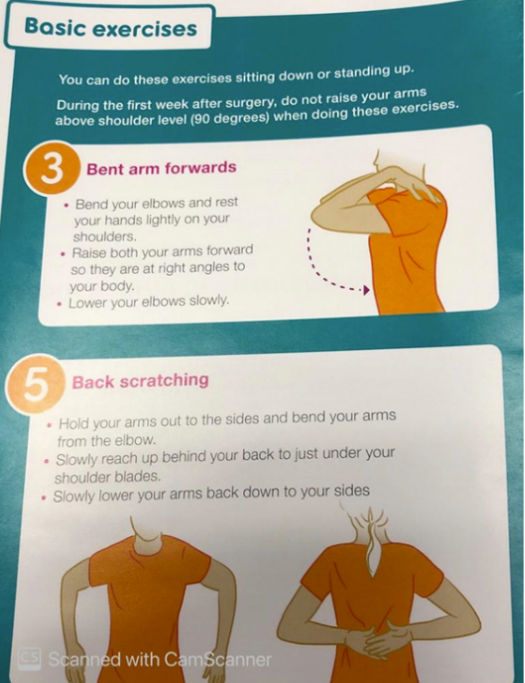
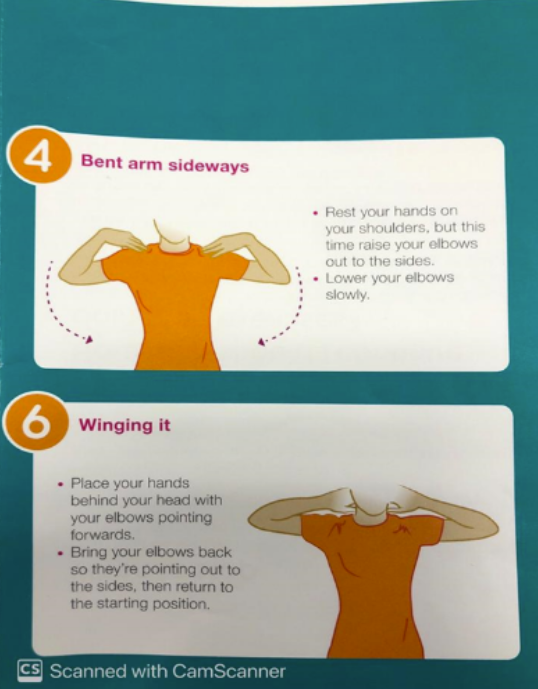
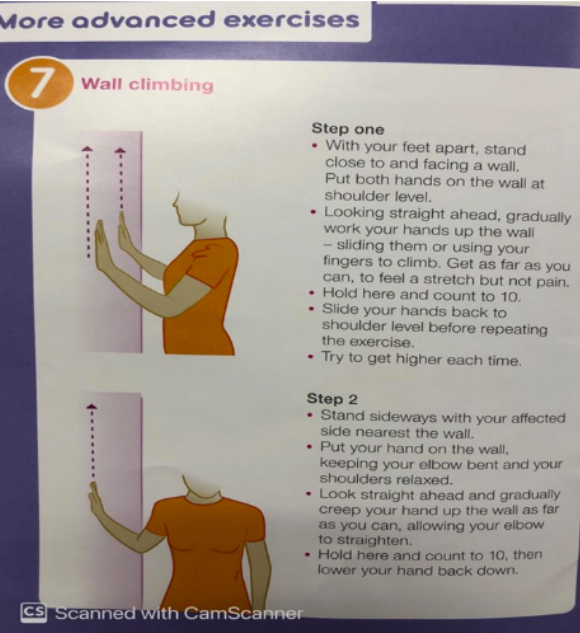
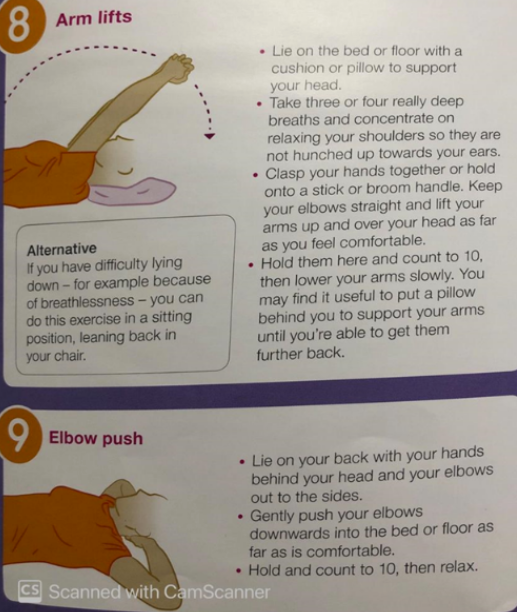
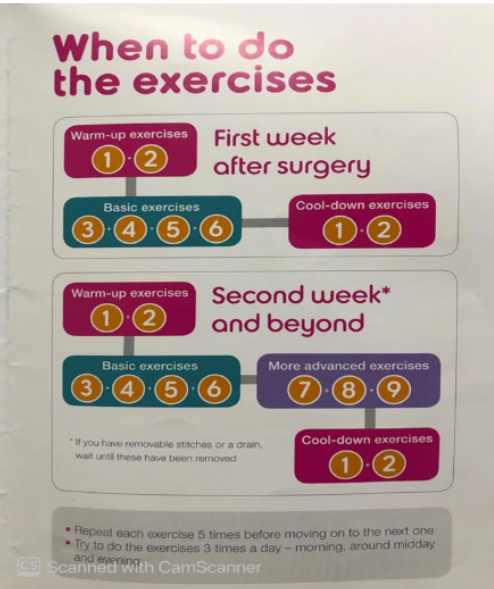
Early postoperative physiotherapy and progressive active and action-assisted shoulder exercises combined with education seem to be effective in prevention of lymphedema after ALND activity of the musculoskeletal pump, increases muscle strength. Exercise may alleviate the lymphedema.
Early detection
breast cancer follow-up routines.
It is recommended to have preoperative measurement of both arms before breast cancer surgery to serve as baseline measurements for further follow-up
Flexibility Exercises
Compressive Garments
- Aim is to limit the fluid accumulation
- Sleeves/gloves/crepe bandages (for mild Lymphedema Stage 0-I)
Decongestive Lymphatic Therapy
DLT is the standard care for moderate to severe lymphedema.
Some of the patients with mild lymphedema might also need intensive treatment if the symptoms are not controlled by compression garments alone.
DLT consists of
MLD


- Multilayer compression bandaging
- Therapeutic exercise
- Skin care
- Properly fitted compression garments
- DLT starts with intensive period ,aiming to reduce the amount of fluid in the tissues.
- Performed 5 times a week but in our clinic...1 session /week for 1 month.
- After each session, the arm is wrapped in a multilayered bandage, therapeutic exercise are advised.....
- After that phase of MLD,when the arm volume is reduced,compression sleeves and gloves are fitted ...maintanance phase..
- DLTcan be repeated at the time of renewing the compression garments.
Surgical Treatment
- Liposuction
- Vascularised Lymph nodes transfer-----Plastic surgery team
- Lymphatico Venous Anastomosis
- Lymphatic Vessels Transplantation
References
- DiSipio T, Rye S, Newman B, et al. Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol. 2013;14:500–15.
- Kwan ML, Darbinian J, Schmitz KH, et al. Risk factors for lymphedema in a prospective breast cancer survivorship study: the pathways study. Arch Surg. 2010;145:1055–63.
- Norman SA, Localio AR, Potashnik SL, et al. Lymphedema in breast cancer survivors: incidence, degree, time course, treatment, and symptoms. J Clin Oncol. 2009;27:390–7.
- McLaughlin SA, Wright MJ, Morris KT, et al. Prevalence of lymphedema in women with breast cancer 5 years after sentinel lymph node biopsy or axillary di
